Wisdom Tooth Removal

What are the symptoms of impacted wisdom teeth?
Should wisdom teeth be automatically taken out if they are healthy?
What is the treatment for painful wisdom teeth or treatment for impacted wisdom teeth?
At what age do wisdom teeth need to be removed?
What are the benefits (indications) for extracting my wisdom tooth?
Who is a suitable candidate for wisdom teeth removal and who is NOT?
What areas do you service as a wisdom tooth surgeon Sydney?
When looking for the best dental surgeon Sydney – what questions should patients ask dental practitioners?
How can training and technique assist in removal of wisdom teeth?
What are the side effects of wisdom tooth surgery?
I’m looking for a mobile wisdom tooth surgeon Sydney – how safe is this service?
How much does wisdom tooth surgery cost?
Am I likely to have wisdom tooth complications?
What is the wait time I will be likely to experience?
What is an impacted wisdom tooth?
- A wisdom tooth is also known as a third molar tooth.
- There is usually one wisdom tooth located on each side (left and right) at the back of both the upper and lower jaws.
- In many patients, the 3rd molar teeth do not erupt into the oral cavity, often because there is not enough space to do so.
- A tooth is considered “impacted” when it has failed to fully erupt into the oral cavity within the expected time frame and can no longer reasonably be expected to do so.

What are the symptoms of impacted wisdom teeth?
The symptoms of an impacted wisdom tooth can vary ranging from many, some or none of the following:
- Jaw pain which may radiate to the temple, ear or neck
- An uncomfortable sensation at the back of the mouth
- A ‘niggling’ feeling
- Feeling of food getting ‘stuck’
- Feeling of something ‘sharp’ at the back of the mouth (if the wisdom tooth is broken)
- Mobile 2nd molar (a loose tooth directly in front of your wisdom tooth)
- Halitosis (smelly breath)
- Localized infections such as pericoronitis which may manifest with intra-oral pain & swelling, limited mouth opening and a foul taste (pus)
- Spreading infections which may manifest as pain and swelling in the face, cheek or neck
- Severe spreading infections (rare) which may manifest with pain and swelling in the neck, difficulty breathing/lying down flat/swallowing, change of character of the voice
It is also possible for a wisdom tooth to be asymptomatic. Even if the wisdom tooth is asymptomatic, it may still have problems that can be detected clinically or radiographically before the above symptoms are likely to develop. These include
- Dental caries (decay)
- Jaw pathology e.g cyst or tumour associated with the wisdom tooth
- Periodontal disease of the 2nd molar tooth (bone loss around the roots of the tooth in front of the wisdom tooth)
Should wisdom teeth be automatically taken out if they are healthy?
The decision to remove a wisdom tooth should be undertaken after an analysis of the potential risks and benefits of this procedure in your clinical situation.
Generally speaking, it is sensible to keep or monitor your wisdom teeth if they are asymptomatic in the following two situations:
- They are erupted and functional in the oral cavity and have an absence of radiographic or clinical disease.
- They are impacted beneath healthy appearing and intact oral soft tissues and have an absence of radiographic disease.
- The management of wisdom teeth involves either extraction or monitoring. If the wisdom tooth requires extraction and is completely or partially buried under gum tissue or bone, then a surgical approach is required to extract the wisdom tooth.
- If the wisdom tooth is painful, associated with infection, or associated with pathology (e.g a cyst) this is unlikely to self-resolve and in these situations, extraction is highly recommended.
- Other common reasons for removing impacted wisdom teeth include decay, periodontal disease, food getting ‘stuck’ in the region & halitosis.
- Wisdom teeth that have no functional value (e.g erupted in the oral cavity but have no tooth opposite to chew on) and are difficult to keep clean, are often also removed in clinical practice.
- Impacted wisdom teeth that are asymptomatic, completely buried beneath healthy appearing & intact oral soft tissues and have no evidence of pathology on an OPG (large jaw X-ray) are very low risk of causing problems in future and are generally managed with monitoring.
At what age do wisdom teeth need to be removed?
- There is no specific age in which wisdom teeth are required to be removed. However, with progressive aging over 25 years old, extraction of wisdom teeth becomes progressively more difficult. This is because with aging, the jaw bones become less elastic (usually necessitating a greater amount of bone removal) and the time taken for the patient to recover after surgery tends to be longer.
What are the benefits (indications) for extracting my wisdom tooth?
Common indications for extracting wisdom teeth include the following
Infection
- Treat an active infection caused by your wisdom tooth which may be localized (e.g. pericoronitis) or spreading to other regions of the head and neck including the airway
- Removal of wisdom teeth with a high probability of developing infections in future
Pathology
- Removal of a wisdom tooth if it is the cause of a cyst or tumor
- Removal of a wisdom tooth if its position is causing trauma to the soft tissues such as the inner surface of the cheeks
- Dental caries (decay)
- Causing pathology of the tooth in front (2nd molar) including dental caries (decay) and periodontal disease (bone loss)
Other
- Wisdom tooth pain
- To improve the oral hygiene status of the mouth
- Halitosis (bad breath)
- As part of an Orthodontic Treatment plan prescribed by your Orthodontist.
Who is a suitable candidate for wisdom teeth removal and who is NOT?
Generally speaking, the majority of patients are suitable for wisdom tooth removal if clinically indicated by an appropriately qualified and trained dental practitioner after the potential benefits and risks are discussed with the patient at the consultation appointment.
The following patients are at a higher risk of a complication from wisdom tooth surgery. In these patient groups, if wisdom tooth surgery is to be offered, it is essential that there is a clear indication for the removal of the wisdom tooth, the patient understands the risks specific to their clinical situation, and the benefits of the surgery are anticipated to outweigh the risks.
- Elderly (> 80years old)
- Immunocompromised
- Radiotherapy to or near the jaw bones
- The wisdom tooth is in close proximity to important anatomical structures such as nerve or sinus
What areas do you service as a wisdom tooth surgeon Sydney?

When looking for the best dental surgeon Sydney – what questions should patients ask dental practitioners?
What is your training in this procedure and where did you train?
How many of these procedures have you done?
What are the side effects of my treatment?
What is your follow up consultation (post operative review) cost?
How can training and technique assist in removal of wisdom teeth?
- Removal of an impacted wisdom tooth is often a difficult procedure which involves advanced surgical techniques such as accessing the bone through incisions of the oral soft tissues, drilling away bone, sectioning teeth, smoothening bone, intra-oral suturing along with the expertise to avoid nearby anatomical structures such as important nerves, blood vessels and the air sinus.
- More qualified and / or experienced practitioners are more likely to make smaller incisions to access the tooth along and handle the surgical flap in a more precise and careful manner which minimizes the post-surgical swelling, bruising and discomfort.
- Patients undergoing oral surgical procedures by more qualified and/or experienced dental practitioners are also thought to be less likely to experience a complication.
- The majority of general dental practitioners would not feel comfortable removing an impacted wisdom tooth/teeth without additional training.
- The decision as to which type of practitioner you want to see to have your wisdom tooth removed is completely up to you.
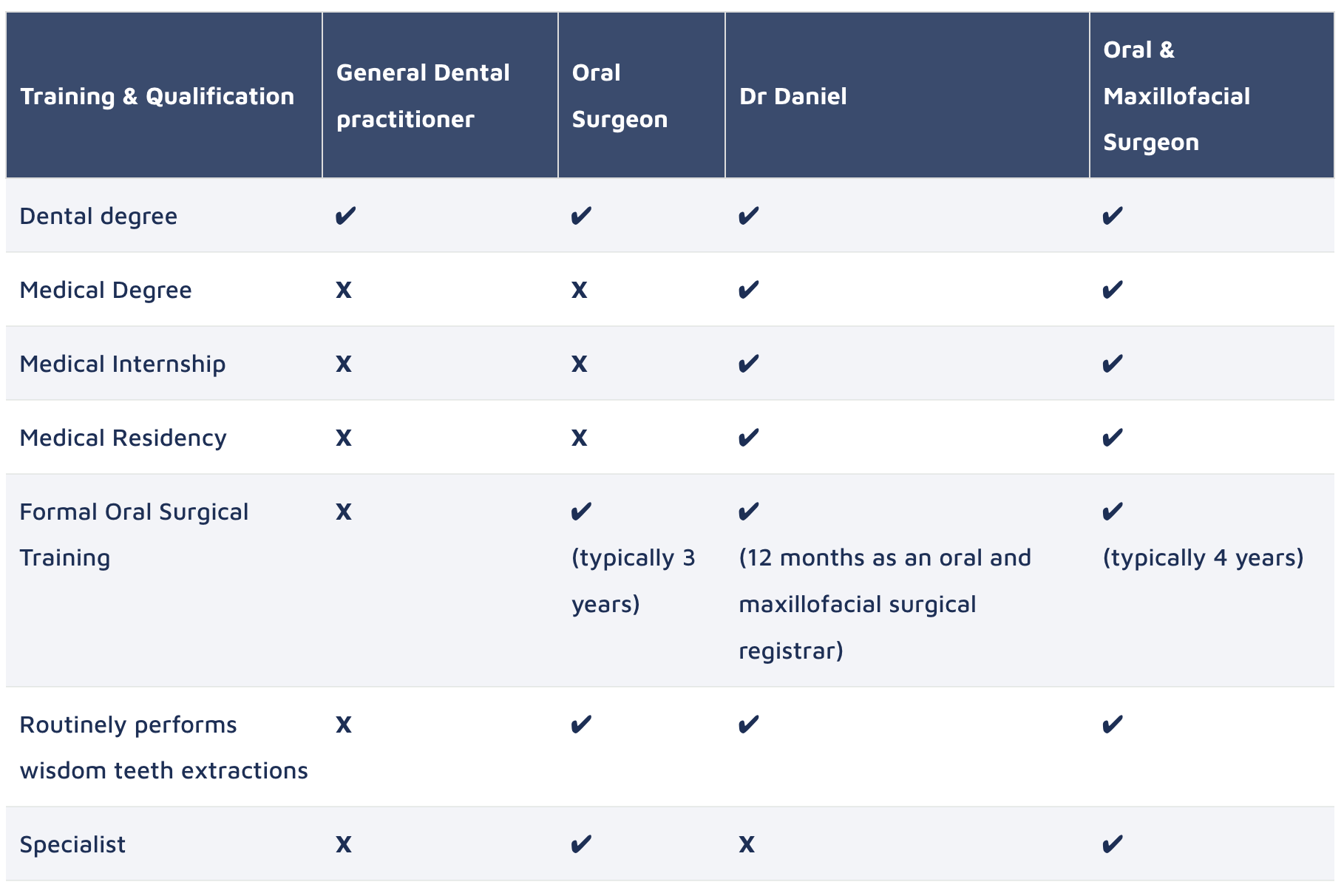
- The following table provides a comparison of the qualifications and training of general dentists, oral surgeons, oral and maxillofacial surgeons to provide you with the information to make an informed decision.
Comparison of the Training & Qualifications of various Dental Practitioners who perform dental extractions*
*This table represents the training pathway in general that each Australian registered dental practitioner would have undertaken.
There will be variations between individual practitioners depending on what additional training & qualifications each may have undertaken. In addition, while specialists generally charge more than generalists, there will be variability in the cost of the procedure between individual clinicians.
What are the side effects of wisdom tooth surgery?
You are likely to experience some or many of the following symptoms and signs after the procedure which are likely to become worse in the next three days as part of the body’s normal healing response to surgery, before you start to feel better and make a full recovery in 2-3 weeks.
- At and near the site of the extraction
- Soreness
- Swelling
- Bruising
- Slow bleeding which is easily controlled by biting down on a rolled piece of gauze for 1hr
- At the jaw joints
- Discomfort at the jaw joint
- Limited mouth opening due to soreness
- General
- Tiredness / fatigue
I’m looking for a mobile wisdom tooth surgeon Sydney – how safe is this service?
- Dr Daniel will be performing your wisdom tooth surgery and the happy gas sedation procedure.
- He is dual qualified in medicine and dentistry and has undertaken 12 months of oral surgical training under the purview of the Oral and Maxillofacial Surgical Unit at a registrar level at Prince of Wales Hospital.
- He routinely performs a high volume of wisdom tooth surgery under happy gas sedation with excellent results.
- At your consultation appointment, you will be assessed for the safety of the wisdom tooth surgery and happy gas sedation procedure, and will only be offered these procedures if an excellent and safe result is anticipated.
- In some situations when the wisdom tooth has to be removed (e.g severe pain or spreading infection in into the face), but there are significant risks of the procedure in your specific clinical situation, you will be informed of the potential risks and the decision as to whether or not you would like to proceed with the surgery is completely up to you.
How much does wisdom tooth surgery cost?
- The prices for surgery depends on the type and complexity offered and a formal quote will be provided at the consultation appointment. Consultation appointments are held by teleconsult for 20 min and has a fee of $90.
Am I likely to have wisdom tooth complications?
- Regardless of surgical discipline, every surgical procedure is associated with potential risks.
- The table below is not exhaustive, but includes the most significant potential complications of wisdom tooth surgery that you need to be aware of.
- The probability of a complication occurring depends on many variables including your age, medical history, surgical difficulty, experience of the operator and patient compliance with the prescribed post operative instructions.
- Dr Daniel will discuss the potential risks of the surgery with you that are specific to your clinical situation and will only offer you wisdom tooth surgery if he believes that the potential benefits of the surgery outweighs the potential risks.
- Dr Daniel performs wisdom tooth surgery routinely with excellent outcomes.
| Complication | Risk factors | Management |
|
Nerve damage
(Applicable to lower wisdom teeth only) |
The proximity of the tooth to the inferior alveolar nerve (sensation to chin, lip and teeth) or lingual nerve (sensation of taste). This sensation may be lost or altered and may be temporary or permanent. |
The key to management is prevention. A 3D scan (CBCT) might be needed to assess how close the tooth is to the nerve and help plan the surgical approach. If occurs, often self-resolves in 3-6months. If the sensation is altered permanently, you may require a referral to a Neurologist for further management. If sensation loss is permanent, the treatment options are limited. |
|
Oral-antral communication [OAC]
(Applicable to upper wisdom teeth only) |
If the upper wisdom tooth is close to the maxillary sinus, a hole between the oral cavity and maxillary sinus may form once the tooth is extracted. |
If the OAC is small, then it will heal itself. If the OAC is large, then it may need a surgical procedure to close it. |
| Incomplete extraction or displacement of part of the tooth to a nearby anatomical space | Difficult anatomy of the tooth such as a curved root or proximity to important structures such as nerves, blood vessels or the air sinus. | If the risk of completing the extraction outweighs the benefit, a small part of the tooth may be left in situ and monitored, usually with periodic radiographs. In the majority of cases, this does not pose any problems for the patient. |
| Bleeding |
On medication that thins the blood (e.g aspirin, warfarin) Medical conditions that pre-disposes to bleeding |
If occurs, is usually mild and well controlled by placing rolled gauze onto the surgical site and biting down firmly for 1hr. In rare instances you might need another surgical procedure to control the bleeding. |
| Infection |
Smoking, diabetes, poor oral hygiene. Medical conditions or medications that suppress the immune system. |
If occurs, is usually mild and responds to conservative management with a short course of oral antibiotics and a chlorhexidine mouthwash. Rarely, another procedure might be need to clean the extraction site, debride bone or incise and drain pus. |
What is the wait time I will be likely to experience?
- The wait time depends on the availability of yourself, the dental practice chair and the Mobile Oral Surgery Services practitioner.
- Generally speaking, if the patient and dental chair are available, Mobile Oral Surgery Services can arrange your consultation within 1 week, and your surgery date under happy gas sedation within 2-3 weeks after your consultation.
- Shorter times for surgery may be possible in emergency situations (pain or swelling).
- Please note patients wishing for IV sedation instead of happy gas sedation will be placed on a wait list.